We now come to how I used (and Kal experienced using) epinephrine for the first time. If you’ve read my previous posts, you understand our experience participating DBV Technology’s REALISE Peanut Patch Trial, and what we did to maintain Kal’s peanut tolerance once the trial ended. Please read those posts for context before continuing.
Part 1
Part 2
When we left off, Kal was eating one Reese’s Piece every day as an oral peanut dose, to maintain his peanut tolerance. Our plan was to gradually increase his doses until he was consuming roughly one peanut daily (3-4 Reese’s Pieces.) We would then maintain that dose.
Unfortunately, we didn’t get that far.
For about two weeks, Kal managed to eat his single Reese’s Piece daily. Some days, he didn’t experience any symptoms at all. Others, he felt a little mouth itchiness or stomach pain. But, apart from the one day when he played too hard and took a hot shower, symptoms remained manageable. We settled dosing into our daily routine.
Queasiness
Then one day in the second week, Kal reported some queasiness in the morning. I didn’t think much of it–I figured he was just tired and hungry. (I know that I’ve felt queasy some mornings when I haven’t had enough sleep, and we usually struggle with sleep at the beginning of the school year.)
Then another day he reported queasiness while playing outside. And then another. One evening, Kal came running in from playing outside and retched a little in the sink. He was fine after rinsing his mouth out, but this was becoming a pattern.
Then Kal reported feeling queasy at school. And because nausea is a possible symptom of COVID-19, they sent him home and said he couldn’t come back without a negative Covid test.
In addition to scheduling a COVID-19 test for Kal, I also called the research hospital. Kal’s queasiness was not in the three-hour window following his doses, but the doctor had mentioned the possibility of chronic GI symptoms. I had assumed he was referring to intestinal upset, but now I wondered if chronic queasiness/nausea could be related to peanut dosing?
Kal’s COVID-19 test came back negative, and the doctor confirmed that the nausea could be related to oral peanut dosing. I was in the process of getting a note for Kal’s school nurse to that effect, but then Kal threw us a curve ball. He threw up.
A stubborn stomach bug
A trip to the doctor told us that Kal had a stomach bug. But it wasn’t short-lived, like most stomach bugs we’ve had. Kal continued throwing up daily (sometimes multiple times daily) for a week. He acted sick for the first few days of actually throwing up, but after that he behaved perfectly normally, except for the few minutes right before and after vomiting.
I returned to the doctor after a week of vomiting, trying to figure out what was ailing my son. The doctor thought it was probably Functional Abdominal Pain. If Kal’s vomiting persisted, he would want to run additional tests. But that’s another matter.
Fortunately, Kal’s vomiting finally stopped after about 10 days. He continued to report queasiness for a few days following that, and then finally seemed normal.
But then we had to reconsider peanut dosing.
OIT and vomiting
When Kal first started his oral peanut dosing, we were told not to dose if he had a fever or if he was vomiting. That meant that we had stopped dosing for the duration of his stomach bug/Functional Abdominal Pain.
They also told us that if Kal missed more than two doses, we needed to check in with the clinic to discuss. He could lose his tolerance if he stopped for too long. We had to be careful when resuming dosing. I didn’t bother calling while Kal was in the midst of his illness. He was missing too many days, but there was nothing we could do about it at the time.
I wasn’t comfortable trying to dose Kal immediately following the vomiting, either. Not while he still felt queasy. His stomach had already been through enough, and stomach pain was his main side effect to the dosing. So I didn’t contact the clinic until both his vomiting and his queasiness were finally over.
Due to a technical difficulty, it took a few more days before I finally connected with the doctor. I was curious whether the peanut dosing could have contributed to Kal’s stomach ailment. But I also wondered if and how we could resume peanut dosing.
I was worried that it was too late.
One more try
The doctor considered the idea of the dosing contributing to Kal’s ailment, but concluded that it should have cleared up faster if that was the case, because we’d stopped dosing right away. He said we could try to resume dosing, but since we had taken so much time off, Kal would have do another in-office food challenge first.
He also said we could just call it quits if we wanted to. If we ever wanted to resume again (say, after Covid vaccines are available so the school won’t send Kal home for every little tummy upset) then we would have to start from scratch. He pointed out that Palforzia was available and that he could see us through it at a later time, or possibly our regular allergist could too.
I asked Kal what he thought. Considering his earlier reluctance, I was surprised and proud of him for wanting to give it one more chance. He said he wanted the dosing to work. So we scheduled one more food challenge.
Coincidentally, one of Kal’s classmates was out with a possible case of COVID-19, so the whole class was on quarantine and doing remote learning. This added to the already-lengthy break Kal had from dosing–we had to wait another week before we could go to the clinic.
Kal’s Final Peanut Challenge
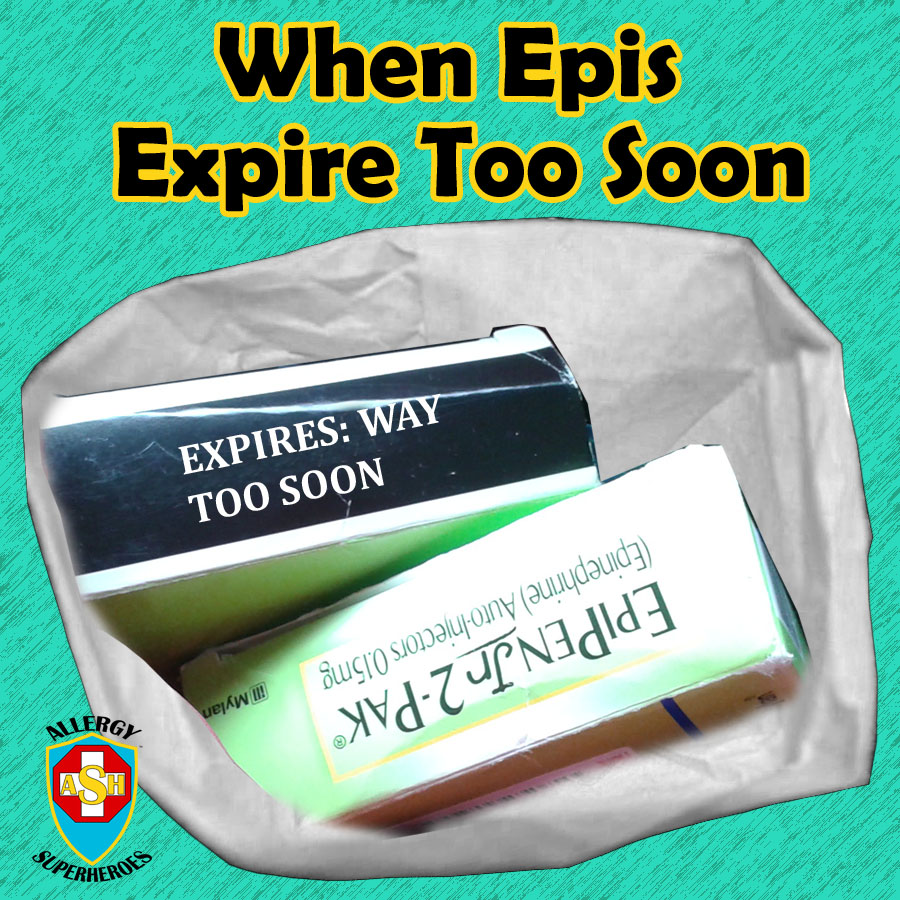
Finally, a month after we’d stopped dosing for the vomiting, Kal was back in the clinic for another peanut challenge. He knew the drill this time and we got started quickly. Kal ate his single Reese’s Piece, once again in ice cream, and we settled down to wait.
It took 15 minutes before Kal reported any symptoms this time, beginning with an itchy tongue. From there it turned into stomach pain which started mild, but slowly progressed to bad. 90 minutes after eating, he reported that his stomach ranked a “10” on a pain scale of 1 to 10.
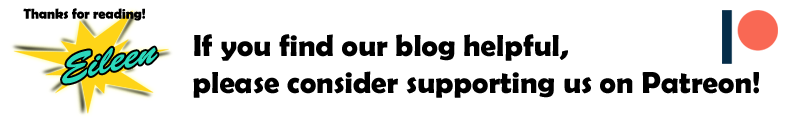
The doctor said we could try to treat it with Zyrtec and heat, but he wasn’t sure if the Zyrtec would do much for the cramping. If that didn’t work, we would use epinephrine. At this point, we knew that Kal wouldn’t be eating daily doses anymore. His peanut tolerance was already gone.
We waited another half hour. Kal’s vitals remained steady, but his cramping cycled up and down. Unfortunately, it never abated so during another “10” cycle, we decided to Epi.


Using Epinephrine
The doctor and nurse brought in an EpiPen and told Kal that he could use it, I could use it, or they could. He said he wanted me to. They weren’t in a hurry, so they rolled up his pant leg and swabbed his skin for a more sterile injection. I tried to convince Kal to put his hand on top of mine so he would have the “empowering” experience of helping himself, but he wasn’t on board with that.
Even though I’ve been anaphylactic for 38 years, this was the first EpiPen I have ever administered into a human.

Some people claim that the EpiPen doesn’t hurt at all.
Even though I’ve never used one, I have always found this claim to be dubious. It’s a needle, after all, and it is injected with a fair amount of force. It’s going to feel like a needle.
I think this claim is largely relational to the symptoms the patient is experiencing. When you’re gasping for air, you’ll barely notice a needle stick compared to the relief of being able to breathe again.
In our case, Kal was in a lot of pain but was nowhere near critical. He yelped and favored his leg all evening. I’m hoping the memory of the relief will overshadow the memory of the needle pain, but I can’t be sure.
Epinephrine Relief
Within five minutes, Kal reported that his stomach pain was half of what it had been before. Within 20 minutes, it was almost gone. We see it again and again, and now my kiddo has experienced it–epinephrine works, and it works fast!
Kal also got very jittery following the EpiPen. I thought it was funny that he described this as “I’m vibrating!”
We remained at the clinic for two hours after the epinephrine dose. Kal’s stomach pain never completely disappeared, and he even said it started to get a little worse again before we left. The doctor told us that we could give him more antihistamine at bedtime and to monitor him, but he didn’t think Kal would need any further epinephrine.
Kal was nervous, but remained brave through it all. He crashed once the epinephrine wore off and was tired for the rest of the evening. Having a severe allergic reaction makes for a long day. He managed to eat a full dinner though, and felt normal in the morning.

The First Time for Epinephrine
A lot of people have asked me if it was scary to use the EpiPen.
I’ll admit that I’ve been scared of it from time to time. As a child, I was scared of the EpiPen after my father took one apart and I saw the size of the spring. That sucker was huge, and I could barely compress it. The thought of a needle jabbing me with that kind of force was scary–and I was pretty good with needles in general.
As an adult, I’ve been more scared of what using the EpiPen means. Using epinephrine means admitting that a reaction is serious, and also that your day is shot. Whatever you planned or hoped to do, you are now going to the Emergency Room instead. I know that’s kind of silly. If you’re considering using epinephrine, the reaction is already serious and your plans are already shot. But somehow, Epi seems to acknowledge and solidify both of these facts. Epi makes it more real.
But in this particular moment, I didn’t feel scared. I’d already decided, more than a month before, that I would give Kal epinephrine under these conditions. And the doctor had already declared, 30 minutes previously, that Epi was the next step. Rather than making me nervous, the action felt kind of inevitable. I’d made it 38 years without using one (except for experiments or practice.) It seemed impractical to think I’d make it a lifetime without ever needing to.
And I’m glad I did it. It’s so very simple, and over so quickly. Many say they’re less afraid of using Epi again once they’ve done it once. I can’t speak for Kal, but I think I feel more ready to use it again, if I need to.
Recovery
It seems kind of silly, but I carried the cap of that EpiPen around in my pocket for the rest of the day. In fact, it’s still in the pocket of that sweater. I’m usually the last member of our family to hoard things, but I feel like I don’t want to get rid of it.
Kal has bounced back remarkably well. The next day, I asked him how he felt about everything. He said he was glad it was over, but disappointed that he can’t keep dosing. I think that sums it up for the rest of us as well.
At least we no longer have to restrict his playing in the evenings.
Hubby and I have been slowly removing the “evidence” of his oral dosing days, by eating up the rest of the Reese’s Pieces. Early on, he decided he didn’t like the taste of peanut butter, so we were always looking for other ways to mask the flavor. He’d eaten Reese’s Pieces in ice cream, yogurt, pressed on top of cookies, and buried in fondant. Hubby and I had to finish off some fondant balls that still had Reese’s in the middle.
Life goes on
So now, nothing changes.
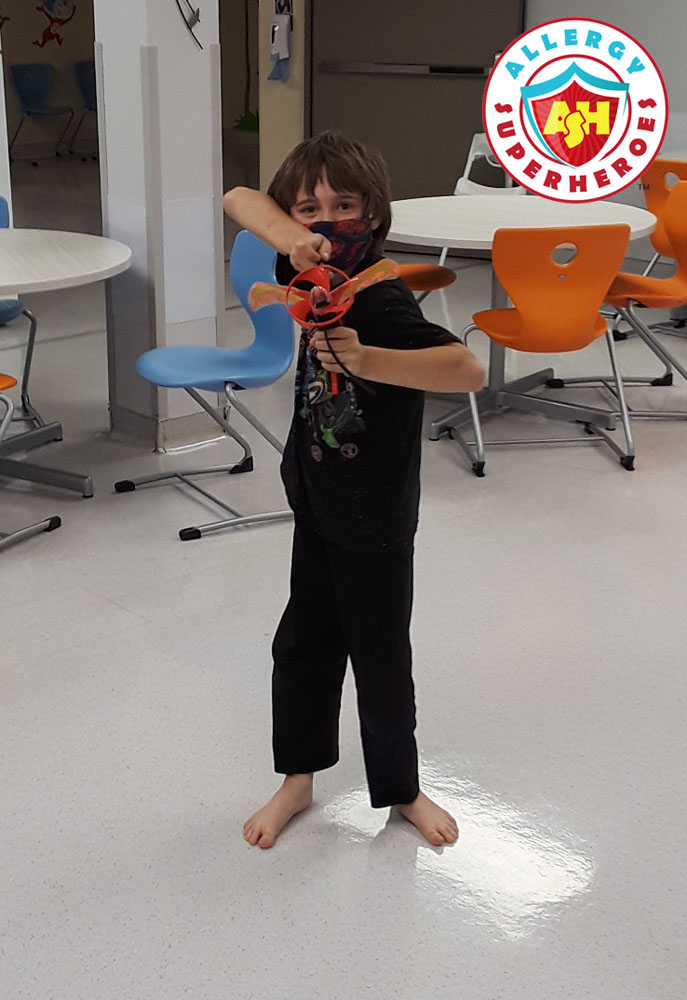
Kal still avoids peanut. I still carry his epinephrine, and he wears a belt pouch with epi-trainers, as practice for when we shift him to the real thing. We still read all labels–another responsibility 9-year-old Kal is beginning to take upon himself. Nothing changes.
Except that things did change.
For three and a half years, we put patches on Kal’s back every night. That was 1/3 of his life. We were building his tolerance. We maintained it for weeks post-trial.
Kal actually ate and tasted peanut. That’s a remarkable achievement. And it’s amazing and sad how quickly all that work got erased.
Hubby’s phone alarm still goes off every evening at 7:00pm, reminding us to change the patch. He hasn’t erased it because we’ve turned it into a fun little ritual. The alarm sound is the James Bond theme, so now instead of changing a patch, everyone in the house pretends to be James Bond and fires a finger gun in a random direction in time with the music.
Sometimes it’s the silly, little things that carry us through.